Medical management of head injuries/concussion is evolving. In recent years, there has been a significant amount of research into concussion in school-aged children especially when participating in sports. HEC has established this protocol for staff and school personnel to provide education and guidance about head injuries and concussion. This protocol outlines procedures for staff to follow in managing head injuries, and outlines school policy as it pertains to return to play/gym.
HEC seeks to provide a safe return to activity for all students after injury, particularly after any head injury. In order to effectively and consistently manage these injuries, procedures have been developed to aid in ensuring that head injured/ concussed students are identified, treated and referred appropriately, receive appropriate follow-up care and academic assistance, and are fully recovered prior to returning to activity.
All staff will attend a yearly online training in which procedures for managing these injuries are reviewed.
Contents:
I. Recognition of head injuries/concussion
II. Management and referral guidelines for all staff
III. Follow-up care during the school day
IV. Guidelines and procedures for coaches
V. Return to play procedures
I. Recognition of concussion
A. Common signs and symptoms of concussion
Signs (observed by others):
• Student appears dazed or stunned
• Confusion (about assignment, plays, etc.)
• Forgets plays or personal details
• Unsure about game, score, opponent, class, staff or peers
• Moves clumsily (altered coordination)
• Balance problems
• Change from baseline or typical mood and behavior
• Responds slowly to questions
• Forgets events that occurred before hitting head
• Forgets events that occurred after hitting head
• Loss of consciousness (any duration)
Symptoms (reported by student):
• Headache
• Fatigue, drowsiness
• Nausea or vomiting
• Double vision, blurry vision
• Sensitive to light or noise
• Feels sluggish
• Feels “foggy”
• Problems concentrating
• Problems remembering
• More emotional than usual
Concussion DANGER SIGNS:
• One pupil larger than the other
• Drowsy or unable to wake up
• Worsening headache
• Weakness, numbness
• Repeated vomiting or nausea
• Slurred speech
• Seizures
• Unable to recognize people or places
• Increasing confusion, restlessness or agitation
• Loss of consciousness
These signs and symptoms are indicative of probable concussion. However, other causes for symptoms should also be considered.
II. Management and Referral Guidelines for All Staff
A. Suggested Guidelines for Management of Head Injury/Concussion
1. Any student with a witnessed loss of consciousness (LOC) of any duration should not be moved and transported immediately to nearest emergency department via emergency vehicle.
2. Any student who has symptoms of a concussion, and who is not stable (i.e., condition is changing or deteriorating), is to be transported immediately to the nearest emergency department via emergency vehicle.
3. A student who exhibits any of the following symptoms should be transported
immediately to the nearest emergency department, via emergency vehicle.
a. deterioration of neurological function (E.g., difficulty responding to verbal stimulation, inability to follow commands, decreased muscle tone, and abnormal movements)
b. decreasing level of consciousness
c. decrease or irregularity in respirations/breathing
d. decrease or irregularity in pulse
e. unequal, dilated, or nonreactive pupils
f. any signs or symptoms of associated injuries, spine or skull fracture, or bleeding (E.g, bleeding or clear drainage from ears or nose, pain in head or neck, inability to move extremities)
g. mental status changes: lethargy, difficulty maintaining alertness, confusion or agitation
h. seizure activity
4. A student who is symptomatic but stable, may be transported by HEC staff. Staff should consult with the nurse on duty/call as to the place of care (primary care physician, or the nearest emergency department). The student’s guardian should be notified about the injury and the plan of treatment.
III. CARE OF THE STUDENT DURING THE SCHOOL DAY
A. Responsibilities of the school nurse after notification of student’s head injury/concussion
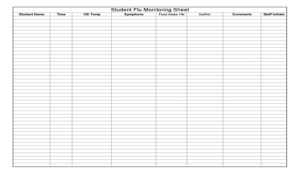
1. Evaluate the student utilizing a graded symptom checklist every 15 minutes for at least 30 minutes.
a. provide an individualized health care plan based on both the student’s current condition, and initial injury information
2. If signs and symptoms are present, refer the student to appropriate medical personnel right away. Send a copy of the checklist.
3. If signs and symptoms are not present, the student can return to class but not to physical activity. Continue to observe student in residence and school for any changes. Notify the nurse of any changes immediately.
4. Notify the student’s guardian of the injury and plan of treatment.
5. Monitor the student on a regular basis. Communicate any special accommodations or plans recommended by the physician
IV. Guidelines and procedures for coaches:
RECOGNIZE, REMOVE, REFER
A. Recognize concussion
All coaches should become familiar with the signs and symptoms of concussion
that are described in section I.
B. Remove from activity
If a coach suspects the athlete has sustained a concussion or exhibits signs or symptoms, the athlete should be removed immediately from activity until evaluated medically. The athlete should not return to physical activity that day.
C. C. Refer the athlete for medical evaluation
Coaches should report all head injuries to the nurse on duty/call, as soon as possible, for medical assessment, management, and coordination of instructions for follow-up care.
If at an away contest, Coaches should seek assistance from the host site medical personnel. Review any recommended treatments with HEC nurse by phone. The student’s guardian should be notified.
a. If there is any question about the status of the athlete, or if the athlete cannot be monitored appropriately, the athlete should be referred to the emergency department for evaluation. A staff should accompany the athlete and remain with the athlete until treatment is completed.
b. Athletes with suspected head injuries should not be permitted to enter the game even if they are not having any symptoms.
V. RETURN TO PLAY (RTP) PROCEDURES AFTER CONCUSSION
A. Returning to participate on the same day of injury
1. As previously discussed in this document, a student who exhibits signs or symptoms of concussion, should not be permitted to return to play or other activities on the day of the injury.
2. “When in doubt, hold them out.”
B. Return to play after concussion
1. The student must meet all of the following criteria in order to progress to activity:
a. Asymptomatic at rest and with exertion (including mental exertion in school) AND:
b. Have written clearance from primary care physician or specialist.
2. Once the above criteria are met, the student will be progressed back to full
activity following a stepwise process.
3. Progression is individualized, and will be determined on a case by case basis by the nurses.
Factors that may affect the rate of progression include:
• previous history of concussion,
• duration and type of symptoms,
• age of the student, and
• sport/activity in which the student participates.
A student with a prior history of concussion, one who has had an extended duration of symptoms, or one who is participating in a collision or contact sport should be progressed more slowly.
4. Stepwise progression:
a) No activity – do not progress to step 2 until the student has absolutely NO symptoms
b) Light aerobic exercise like walking or riding a stationary bike; if no symptoms then progress to “c”
c) Sport-specific training and gym class which is an increase in activity (e.g., playing basketball, running in soccer or participating in gym); if no symptoms- progress to “d”
d) Non-contact training drills or activity for extended periods of time; if no symptoms-progress to full activity
e) Full-contact training and activity after medical clearance and absence of any symptoms
Note: If the student experiences post-concussion symptoms during any phase, the athlete should drop back to the previous asymptomatic level and resume the progression after 24 hours.
Remember the symptoms you might observe and would prohibit advancement of activity are:
headache, fatigue, drowsiness, nausea, blurry vision, feeling sluggish or “foggy,” problems concentrating in class or problems remembering.
Call the nurse if any symptoms reoccur.
D. Seizure
What to DO During a Seizure:
1. Keep Calm. Ease the person to the floor, if they are standing or sitting. (If in bed, do not move).
2. If possible, clear the area of other students, non-essential staff and obstacles.
3. DO NOT restrain the child’s movements. Loosen his / her clothing. Keep him / her away from any harmful objects. DO NOT force his / her mouth open. DO NOT force anything between his / her teeth. If possible turn the child on his / her side to release secretions from mouth. Observe neck precautions if there is any possibility of head trauma.
4. Treat the occurrence matter-of-factly, and explain to the other children / staff that there is no danger, that the child will not hurt him / herself, and that the seizure will be over in a few minutes.
5. After the seizure stops, and the child appears to be relaxed, let him / her sleep or rest quietly in a place where he / she will not be disturbed.
6. All seizures are to be considered important, and reported immediately to the Nursing Staff.
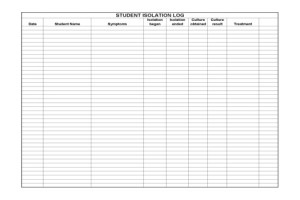
7. In describing the seizure to Supervisory Personnel, staff should try to be as accurate as possible. An accurate description of any seizure is important to the Physician treating the child. There is a form for reporting the event, which is kept in the Supervisor’s Office.
(See Attachment E)
8. EMS should be called:
• If the seizure lasts more than five minutes
The person has one seizure after another without gaining consciousness between episodes if the seizure stops, but the person does not regain consciousness within 10-15 minutes
E. Fever
1. Assess for additional symptoms – level of alertness, respiratory, GI, or GU symptoms, complaints of pain, chills, or the presence of any infected skin lesions.
2. Temperatures above 101 Degrees, should be recorded every 4 hours. Elevated temperatures at or above 103 Degrees, need to be recorded every 3 hours.
3. For temperatures of 101 Degrees and above, administer acetaminophen every 4-6 hours or ibuprofen every 6-8 hours. Encourage increased fluid intake.
4. Notify Physician for any fever over 101 >24 hours OR if there are additional concerning symptoms at any time.
5. A cool washcloth may be applied to the child’s forehead for comfort.
***********************************